Understanding the Importance of Fall Prevention
Preventing falls in elderly individuals is crucial for maintaining their health and independence. This listicle provides eight actionable strategies to reduce fall risk. Learn how strength and balance training, medication management, home modifications, vision correction, proper footwear, fall risk assessments, vitamin D, and assistive devices can significantly improve senior safety. These practical tips empower seniors and caregivers to create a safer environment and prevent falls.
1. Strength and Balance Training Programs
One of the most effective ways of preventing falls in elderly individuals is through targeted strength and balance training programs. These structured exercise programs are designed to improve muscle strength, flexibility, and balance, which are crucial for maintaining stability and preventing falls. They typically involve a combination of resistance training, weight-bearing exercises, and specialized balance activities that challenge and improve the body's stability systems. These programs address the core physical issues that contribute to falls, making them a cornerstone of fall prevention strategies.

Strength and balance training programs incorporate various features to maximize their effectiveness. These include progressive resistance training to gradually build muscle strength, balance-specific exercises like standing on one foot or heel-toe walking, and core strengthening components to improve postural stability. Programs can be delivered in group settings or individually tailored to meet specific needs and preferences. The typical recommendation is for participation 2-3 times per week. For seniors and elderly individuals, these programs offer significant advantages, including improved reaction time, coordination, and overall physical function. The benefits extend beyond fall prevention, contributing to better overall health and well-being. Moreover, these programs can be adapted for different mobility levels, making them accessible to a wider range of seniors, including those with existing mobility challenges. For family caregivers, the improved mobility and reduced fall risk can translate to less intensive caregiving needs and greater peace of mind.
Examples of Successful Programs:
- Otago Exercise Programme: Developed in New Zealand, this program has shown to reduce falls by up to 35%.
- Tai Chi for Arthritis and Fall Prevention: Endorsed by many departments of health, Tai Chi improves balance and coordination through gentle, flowing movements.
- Matter of Balance: This program combines exercise with fear management, addressing both the physical and psychological aspects of fall prevention.
- FallProof™: A comprehensive balance and mobility training program.
Pros:
- Directly addresses physical weakness that contributes to falls.
- Improves reaction time and coordination.
- Has additional health benefits beyond fall prevention.
- Can be adapted for different mobility levels.
- Social aspects when done in groups can improve adherence and provide valuable social interaction.
Cons:
- Requires consistent participation to maintain benefits.
- May require professional supervision initially, particularly for those with pre-existing conditions.
- Some exercises carry their own fall risk if not properly supervised or performed correctly.
- May not be suitable for those with certain medical conditions. Consultation with a physician is crucial.
- Can take several weeks to show significant improvement, requiring patience and commitment.
Tips for Starting and Maintaining a Program:
- Assessment: Start with a physical therapist assessment to identify specific needs and limitations. This is especially important for healthcare professionals working with discharging patients.
- Gradual Progression: Begin with seated exercises if standing balance is poor. Use stable support (like a counter) when starting balance exercises. Gradually increase duration and difficulty as ability improves.
- Consistency: Consistent participation is key to realizing the benefits. Family caregivers can play a crucial role in encouraging and supporting seniors' adherence to the program.
- Combination Approach: Combine strength and balance training with other fall prevention strategies for maximum effectiveness.
Why this approach is essential for preventing falls in elderly:
Falls are a significant health concern for the elderly, often leading to injuries, reduced mobility, and decreased quality of life. Strength and balance training programs directly address the underlying physical factors that contribute to falls, making them a crucial component of any comprehensive fall prevention strategy. For Caring Hands Senior Services' target demographics, this approach is especially relevant. It empowers seniors to maintain their independence and reduces the burden on family caregivers. It also provides healthcare professionals with a valuable tool for improving patient outcomes after discharge. By improving strength, balance, and coordination, these programs not only reduce the risk of falls but also enhance overall physical function and well-being, allowing seniors to live more active and fulfilling lives.
2. Medication Review and Management
A crucial step in preventing falls in elderly individuals is a comprehensive review and management of their medications. This strategy directly addresses a major modifiable risk factor for falls: medication side effects. Many commonly prescribed medications, including those for sleep, anxiety, and high blood pressure, can cause dizziness, drowsiness, lightheadedness, and hypotension (low blood pressure), all of which significantly increase the risk of falling. Therefore, medication review and management is essential for maintaining seniors' safety and well-being and deserves a prominent place on this list.
How it Works:
Medication review and management involves a systematic evaluation of all medications an elderly person is taking, including both prescription and over-the-counter drugs, herbal supplements, and vitamins. This process, ideally led by a physician or pharmacist specializing in geriatric care, aims to:
- Identify Potentially Inappropriate Medications (PIMs): Using established criteria like the STOPP/START criteria and the Beers Criteria, healthcare providers identify medications that may be inappropriate for older adults due to their high risk of adverse effects or safer alternatives.
- Reduce Polypharmacy: Polypharmacy, the concurrent use of multiple medications, is a significant problem among the elderly, increasing the risk of drug interactions and adverse events, including falls. Medication review seeks to streamline medication regimens by deprescribing unnecessary drugs.
- Optimize Medication Dosages: Age-related changes in metabolism and kidney function can affect how the body processes medications. Dosage adjustments may be necessary to ensure safety and efficacy while minimizing side effects.
Features of Effective Medication Review:
- Comprehensive Review: Includes all medications, including over-the-counter drugs and supplements.
- Assessment of Side Effects, Interactions, and Dosages: Careful consideration of potential adverse effects, drug-drug interactions, and age-appropriate dosages.
- Deprescribing: Safely discontinuing unnecessary or potentially harmful medications.
- Consideration of Alternatives: Exploring safer alternative medications with a lower fall risk.
- Regular Scheduled Reviews: Ongoing monitoring (e.g., every 6-12 months) to account for changes in health status and medication needs.
Pros:
- Addresses a major modifiable risk factor for falls.
- Can improve overall health outcomes beyond fall prevention.
- Often reduces medication costs and complexity.
- Non-invasive intervention with potentially immediate benefits.
- Can improve medication adherence and effectiveness.
Cons:
- Requires cooperation between multiple healthcare providers (physicians, pharmacists, etc.).
- May be resistance from patients to changing established medications.
- Potential for withdrawal effects during medication changes (requires careful management by a physician).
- Time-intensive process for healthcare providers.
- Insurance may not cover comprehensive medication reviews.
Examples of Successful Implementation:
- STOPP/START criteria: A screening tool to identify potentially inappropriate prescriptions and prescribing omissions in older adults.
- Beers Criteria: Guidelines for medication use in older adults, highlighting drugs to avoid or use with caution.
- Medication Therapy Management (MTM) services: Provided by pharmacists to optimize medication regimens and improve patient outcomes.
- Veterans Affairs MedSAFE program: Focuses on reducing the use of psychotropic medications in older veterans, which are often associated with increased fall risk.
Actionable Tips for Preventing Falls through Medication Management:
- Maintain an updated list: Keep a comprehensive and current list of all medications, including over-the-counter products, supplements, and vitamins. Share this list with all healthcare providers.
- Schedule regular reviews: Discuss medication management with your physician or pharmacist, especially if you experience dizziness or balance problems. Aim for reviews every 6-12 months.
- Report side effects: Immediately report any dizziness, lightheadedness, or balance changes after starting a new medication.
- Use pill organizers: Pill organizers can improve medication adherence and prevent missed doses, which can contribute to instability and falls.
- Consult a pharmacist: Consider asking for a pharmacist consultation specifically focused on fall risk and medication optimization.
This approach is particularly important for seniors who are experiencing dizziness, have a history of falls, or take multiple medications. By proactively addressing medication-related fall risks, we can significantly improve the safety and well-being of older adults.
3. Home Safety Modifications
One of the most effective ways of preventing falls in elderly individuals is through home safety modifications. This approach involves a systematic assessment of the home environment to identify and remove potential hazards while implementing safety features that minimize fall risk. The goal is to create a living space that supports age-related changes in mobility, vision, and balance, enabling seniors to live more safely and independently. This proactive strategy provides passive protection, meaning it doesn't rely on the senior remembering to take specific actions each time.

Home safety modifications encompass a wide range of adjustments, including:
- Professional Home Safety Assessments: A trained professional, often an occupational therapist, can evaluate the home and provide tailored recommendations for modifications.
- Removal of Trip Hazards: This includes addressing common dangers such as loose rugs, cluttered pathways, and electrical cords. Decluttering can make a home safer and easier to navigate, which is especially important for seniors. For helpful advice on decluttering specifically for seniors, check out this guide on decluttering tips for seniors.
- Installation of Safety Features: Installing grab bars in bathrooms, handrails along staircases, and stair gates can significantly reduce fall risks.
- Improved Lighting: Enhancing lighting, particularly in stairways, hallways, and bathrooms, improves visibility and reduces the likelihood of trips and stumbles.
- Adaptive Equipment: Utilizing adaptive equipment such as raised toilet seats, shower chairs, and bedside commodes can make daily tasks safer and easier to manage.
Pros of Home Safety Modifications:
- Provides passive protection, requiring no active participation from the senior.
- One-time modifications offer ongoing benefits.
- Can be customized to individual needs and specific home layouts.
- May enable seniors to age in place longer, maintaining independence and familiarity.
- Often a relatively low-cost solution compared to the expenses associated with falls and medical interventions.
Cons of Home Safety Modifications:
- May require a significant initial investment, although simpler modifications can be affordable.
- Some modifications may necessitate professional installation, adding to the cost.
- Housing limitations, such as rental properties, may restrict modification options. However, temporary modifications can often be implemented.
- Does not address falls that occur outside the home.
- Can be met with resistance from seniors who are reluctant to change their familiar environment. Open communication and involving the senior in the decision-making process are crucial.
Examples of Successful Implementation:
- CAPABLE (Community Aging in Place—Advancing Better Living for Elders) program: This evidence-based program combines home modifications with other services to help seniors age in place.
- AARP HomeFit Guide: This guide provides practical tips and resources for making homes safer and more livable for older adults.
- Area Agencies on Aging: Many Area Agencies on Aging offer programs that provide home modification services and assistance.
- Australia's Home and Community Care (HACC) program: This program provides funding for home modifications and other support services for seniors.
Actionable Tips for Preventing Falls in Elderly Individuals Through Home Modifications:
- Start with a professional assessment: An occupational therapist can identify specific hazards and recommend appropriate modifications.
- Prioritize high-risk areas: Focus on bathrooms, stairs, and bedrooms first, as these are common locations for falls.
- Use contrasting colors: Enhance visibility by using contrasting colors to highlight edges, steps, and level changes.
- Consider temporary modifications for rentals: Portable grab bars, non-slip mats, and improved lighting can be easily installed and removed.
- Combine with behavioral changes: Encourage habits like keeping frequently used items within easy reach and using assistive devices.
Home safety modifications are a crucial component of a comprehensive fall prevention strategy. By proactively addressing environmental hazards, we can significantly reduce the risk of falls, promote independence, and enhance the overall well-being of elderly individuals. This method deserves its place on the list because it offers a long-term, proactive solution that can significantly reduce fall risk and improve the quality of life for seniors wishing to age in place.
4. Vision Assessment and Correction
Vision plays a crucial role in maintaining balance and preventing falls, especially in the elderly. Age-related vision changes, often overlooked, can significantly increase fall risk. This makes vision assessment and correction a vital component of any fall prevention strategy for seniors. Addressing visual impairments not only reduces the risk of falls but also significantly improves overall quality of life and independence, allowing seniors to remain safe and active in their homes and communities.
How it Works:
This approach focuses on a comprehensive evaluation and management of vision problems that contribute to falls. This includes:
- Regular Eye Examinations: Annual comprehensive eye exams with dilation are crucial for those 65 and older. These exams can detect age-related eye diseases like cataracts, glaucoma, and macular degeneration in their early stages.
- Prescription Updates: Ensuring eyeglasses prescriptions are up-to-date is essential. Changes in vision can occur gradually, and outdated prescriptions can impair depth perception and visual acuity, directly impacting balance.
- Cataract Surgery: When indicated, cataract surgery can dramatically improve vision and has been shown to reduce fall risk by up to 34%.
- Adaptive Strategies: For seniors with permanent visual impairments, occupational therapy and adaptive strategies can help them navigate their environment safely. These strategies might include using magnifying glasses, increasing lighting, and modifying the home environment.
- Assessment for Specific Visual Deficits: Evaluations should specifically assess visual acuity, depth perception, contrast sensitivity, and visual field deficits, as these are all critical factors in maintaining balance and spatial awareness.
Examples of Successful Implementation:
- Cataract surgery: Studies have demonstrated a significant reduction in falls post-surgery.
- VISUALLY program: This program focuses on providing low-vision adaptations for homes, improving safety and independence.
- Royal National Institute of Blind People (RNIB) (UK): The RNIB offers comprehensive vision assessment protocols and resources for those with low vision.
- Specialized occupational therapy programs: These programs offer low vision rehabilitation, teaching adaptive techniques and strategies for daily living.
Actionable Tips for Preventing Falls in Elderly Through Vision Care:
- Schedule annual comprehensive eye exams with dilation.
- Wear single-vision glasses (not bifocals) for outdoor activities and when navigating stairs.
- Increase lighting throughout the home, paying particular attention to transitional spaces like hallways and doorways.
- Use high contrast for important edges, such as stair nosings in contrasting colors.
- Remove or mark glass doors and low-contrast obstacles.
When and Why to Use This Approach:
Vision assessment and correction should be a routine part of preventative care for all seniors, especially those at increased risk for falls. This includes individuals with existing vision problems, a history of falls, or mobility issues. Because vision changes can be subtle and occur gradually, regular assessments are crucial even in the absence of noticeable symptoms.
Pros:
- Addresses a significant and often overlooked fall risk factor.
- Improvement can be substantial and immediate after interventions like cataract surgery.
- Often covered by insurance, including Medicare.
- Benefits extend beyond fall prevention to quality of life improvements.
- Can help identify early signs of other health conditions.
Cons:
- May require specialist appointments that have long wait times.
- Corrective surgeries carry their own risks for elderly patients.
- Adaptive techniques require learning and practice.
- Progressive conditions may require ongoing adaptations.
- Some visual impairments cannot be fully corrected.
Popularized By:
- American Academy of Ophthalmology
- Dr. Cynthia Owsley, researcher in vision and aging
- The Lighthouse Guild for vision rehabilitation
- National Eye Institute's vision rehabilitation initiatives
This focus on vision assessment and correction aligns perfectly with the needs of Caring Hands Senior Services’ target audience, including seniors, family caregivers, and healthcare professionals, by providing a proactive and effective way to address a major fall risk factor and improve the overall well-being of elderly individuals. By integrating these strategies, we can significantly enhance the safety and independence of the seniors in our care.
5. Footwear Assessment and Modification
Proper footwear plays a crucial role in preventing falls in the elderly. This often-overlooked aspect of senior care can significantly impact stability and balance, directly contributing to a reduction in fall risk. Footwear assessment and modification involves evaluating an individual's current footwear and making necessary adjustments to optimize safety and comfort. This strategy is an essential component of any comprehensive fall prevention program, particularly for seniors aging in place or dealing with chronic conditions.
How it Works:
Footwear assessment and modification begins with a professional evaluation of the individual's feet, gait, and current footwear choices. This assessment might be performed by a podiatrist, physical therapist, or other trained healthcare professional. They identify any foot problems, gait abnormalities, or ill-fitting shoes that could contribute to falls. Following the assessment, recommendations are made for appropriate footwear, including specific features like non-slip soles and good heel support. In some cases, custom orthotics may be prescribed to address individual biomechanical issues and improve stability. Regular footwear checks and timely replacements are also essential to maintain optimal foot health and reduce fall risk.
Examples of Successful Implementation:
Several studies and programs highlight the effectiveness of footwear interventions in reducing falls among the elderly. Comprehensive footwear programs in Australian aged care facilities have demonstrated a 30% reduction in falls. The Veterans Administration also utilizes specific footwear assessment protocols as part of its fall prevention strategy. Furthermore, companies like New Balance have partnered with senior living communities to provide footwear education and promote proper footwear choices among residents. Falls Prevention Clinics frequently incorporate podiatric assessments to address foot-related fall risks.
Actionable Tips for Preventing Falls in Elderly through Footwear:
- Choose shoes with a firm heel counter and flexible, non-slip soles: These features provide stability and prevent slipping.
- Avoid backless slippers, high heels, and shoes with smooth soles: These types of footwear offer little support and increase the risk of trips and falls.
- Replace shoes when the tread wears down or support deteriorates: Worn-out shoes compromise stability and increase fall risk.
- Consider athletic shoes with a proper fit for daily wear, even indoors: Athletic shoes often provide better support and cushioning than traditional dress shoes or slippers.
- Have feet measured regularly, as size and shape can change with age: Ill-fitting shoes can negatively impact balance and gait.
- Opt for easy-to-use closures like Velcro: This is particularly helpful for seniors with limited dexterity or arthritis.
Why Footwear Assessment and Modification Deserves its Place on the List:
This relatively simple and cost-effective intervention can be implemented immediately and addresses a direct interface between the body and the environment. It not only improves safety by reducing fall risk, but also enhances comfort and mobility, potentially alleviating other foot-related pain and problems. This is especially important for Caring Hands Senior Services' target demographics, including seniors aging in place, those with chronic conditions, and individuals transitioning from hospital or rehab facilities. Providing proper footwear can significantly improve their quality of life and independence.
Pros:
- Relatively simple and cost-effective intervention
- Immediate implementation possible
- Addresses a direct interface between the body and environment
- Can improve comfort and mobility in addition to safety
- May help with other foot-related pain and problems
Cons:
- May require replacement of existing footwear collection
- Cost of appropriate footwear and custom orthotics can be significant (though often less expensive than a fall-related injury)
- Potential resistance to changing long-standing footwear preferences – education and gentle persuasion are key
- Limited Medicare coverage for therapeutic footwear (primarily for diabetics); exploring supplemental insurance or other financial assistance options may be necessary
- Requires consistent compliance to be effective – ongoing monitoring and support from caregivers and family members are important
Popularized By:
- American Podiatric Medical Association
- Dr. Marian Hannan, researcher in footwear and falls
- Companies like New Balance, Brooks, and Hoka developing senior-friendly footwear
- The Institute for Preventive Foot Health
By prioritizing footwear assessment and modification, Caring Hands Senior Services can make a significant contribution to fall prevention and improve the overall well-being of their clients. This proactive approach aligns with the goal of supporting seniors in maintaining their independence and safely aging in place.
6. Multifactorial Fall Risk Assessment and Intervention
Preventing falls in elderly individuals requires a comprehensive approach that addresses the multiple factors often contributing to these incidents. A Multifactorial Fall Risk Assessment and Intervention is a personalized strategy that identifies and targets these specific risks, leading to more effective fall prevention. This approach recognizes that falls are rarely caused by a single factor but rather a complex interplay of physical, cognitive, and environmental issues. It involves a thorough assessment process followed by a tailored intervention plan, making it a significantly more effective method than addressing individual risk factors in isolation.
This method works by first conducting a comprehensive assessment across multiple domains. This typically includes evaluating the individual's physical health (strength, balance, gait, medication review), cognitive function (memory, judgment, attention), and environmental factors (home hazards, lighting, assistive devices). Standardized risk assessment tools, such as the Morse Fall Scale, STRATIFY, and the Timed Up and Go (TUG) test, are often employed to provide a quantifiable measure of risk. The following infographic visualizes the key data and concepts related to Multifactorial Fall Risk Assessment, illustrating how these elements connect to create a personalized fall prevention plan. The central concept is the individualized fall prevention plan, stemming from the comprehensive assessment across various domains.
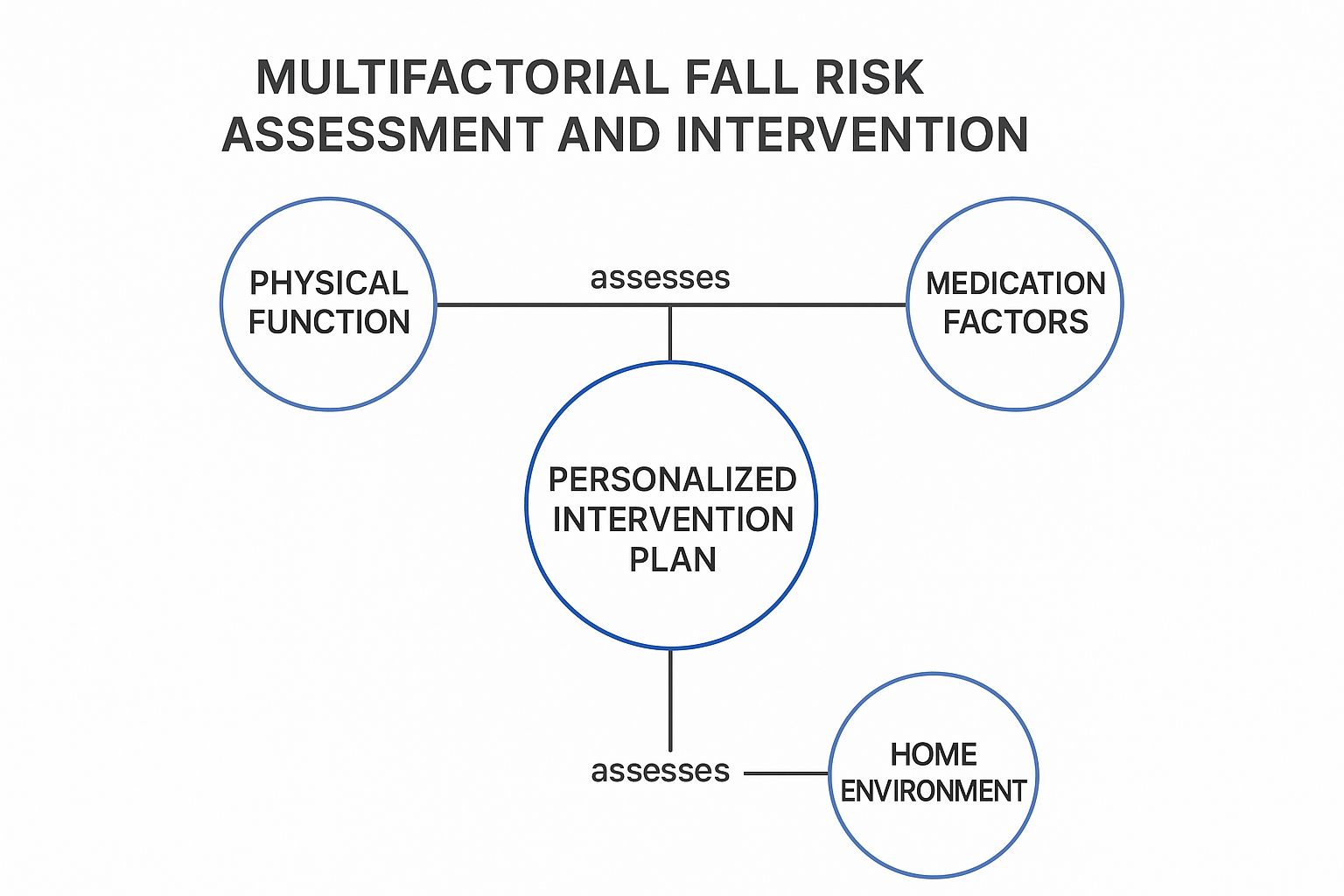
The infographic clearly demonstrates the multifactorial nature of fall risk and how a comprehensive assessment leads to a personalized intervention plan encompassing various aspects of a senior's life. It highlights the importance of considering physical, cognitive, and environmental factors in preventing falls. The convergence of these assessment domains into the tailored plan underscores the integrated approach necessary for effective fall prevention.
Based on the assessment results, a multidisciplinary team, which may include a physician, physical therapist, occupational therapist, nurse, and pharmacist, develops a personalized intervention plan. This plan addresses the identified risks through targeted interventions, such as strength and balance training, medication adjustments, home modifications, and assistive device prescription. Regular reassessments and plan adjustments are essential to ensure the plan's ongoing effectiveness and adapt to any changes in the individual's health or circumstances.
Examples of successful implementations:
- STEADI (Stopping Elderly Accidents, Deaths & Injuries) program by CDC: Provides resources and tools for healthcare providers to implement effective fall prevention programs.
- Yale FICSIT (Frailty and Injuries: Cooperative Studies of Intervention Techniques): A research program focusing on preventing falls and fractures in older adults.
- VA Falls TEAM (Team Evaluation and Assessment of Movement) program: Specifically designed for veterans, this program employs a team approach to fall risk assessment and intervention.
Pros:
- Addresses the multifactorial nature of fall risk comprehensively.
- Individualized approach increases effectiveness.
- Coordinates efforts across healthcare providers.
- Has shown up to 24% reduction in fall rates in studies.
- May identify previously unrecognized health issues.
Cons:
- Resource-intensive and potentially expensive to implement fully.
- Requires coordination across multiple providers and services.
- Time-consuming for both providers and patients.
- May have inconsistent insurance coverage.
- Challenging to implement outside integrated health systems.
Tips for readers:
- Start with a primary care provider to coordinate referrals.
- Keep a falls diary to identify patterns and triggers.
- Prioritize interventions based on the most significant risk factors.
- Follow through with all components of the program for best results.
- Request regular reassessments, especially after health changes.
This multifactorial approach deserves a prominent place on this list because it offers the most comprehensive and personalized strategy for preventing falls in the elderly. While single-factor interventions can be helpful, addressing the multifaceted nature of fall risk through this method significantly increases the likelihood of success and promotes overall well-being. This approach aligns perfectly with Caring Hands Senior Services' commitment to providing comprehensive and individualized care for seniors, empowering them to maintain their independence and quality of life. By incorporating multifactorial fall risk assessments, Caring Hands can proactively address fall risks and contribute to a safer and healthier environment for their clients.
7. Vitamin D Supplementation
Vitamin D plays a crucial role in muscle function and bone health, both essential for preventing falls in the elderly. As we age, our bodies become less efficient at producing vitamin D from sunlight, and dietary intake often falls short. This can lead to deficiencies that contribute to muscle weakness, poor balance, and an increased risk of falls. Therefore, strategic vitamin D supplementation is a valuable tool in a comprehensive fall prevention strategy, especially for seniors. This approach involves testing vitamin D levels, prescribing appropriate supplements, and regular monitoring to optimize effectiveness.
How Vitamin D Supplementation Works:
Vitamin D supplementation addresses deficiencies by providing the body with this essential nutrient directly. It works by:
- Improving muscle strength: Vitamin D receptors are present in muscle tissue, and adequate levels are essential for optimal muscle function.
- Enhancing bone health: Vitamin D promotes calcium absorption, which is vital for maintaining strong bones and reducing the risk of fractures, a common cause of falls and subsequent complications in seniors.
Features of a Vitamin D Supplementation Program:
- Assessment of vitamin D levels: A simple blood test (25-hydroxyvitamin D) is necessary to determine existing deficiency levels.
- Personalized supplementation: Dosage is prescribed based on the individual's deficiency and overall health status.
- Regular monitoring and dose adjustment: Follow-up blood tests are important to ensure optimal levels are maintained and to adjust dosage as needed.
- Consideration of calcium co-supplementation: Calcium and vitamin D work synergistically for bone health, and co-supplementation may be recommended.
- Education: Patients receive information about dietary sources of vitamin D and safe sun exposure practices.
Benefits of Vitamin D Supplementation for Preventing Falls in Elderly:
- Relatively simple and low-cost intervention: Vitamin D supplements are readily available and generally affordable.
- Addresses a common deficiency in elderly populations: Many seniors are deficient in vitamin D, making supplementation a widely applicable strategy.
- May provide benefits beyond fall prevention: Adequate vitamin D levels are linked to improved bone health, immune function, and overall well-being.
- Can be implemented alongside other strategies: Vitamin D supplementation complements other fall prevention methods, such as exercise and home modifications.
- Minimal side effects when properly dosed: Side effects are rare when vitamin D is taken at recommended doses.
Potential Drawbacks:
- Effectiveness may be limited to those with deficiency: Supplementation may not significantly reduce fall risk in individuals with already adequate vitamin D levels.
- Research shows mixed results on fall prevention effectiveness: While some studies have shown promising results, others have shown limited impact. The effectiveness of vitamin D supplementation for fall prevention remains a topic of ongoing research.
- Requires blood testing for proper dosing: Initial and periodic blood tests are needed for accurate monitoring.
- Potential for toxicity with very high doses: Excessive vitamin D intake can be harmful, highlighting the importance of proper dosing and monitoring.
- May interact with certain medications: It is crucial to inform your healthcare provider about all medications being taken to avoid potential interactions.
Examples of Successful Implementation:
- A systematic review showed a 19% reduction in fall risk with vitamin D supplementation in deficient individuals.
- The USPSTF provides recommendations on vitamin D supplementation for community-dwelling adults 65 and older.
- Finland's vitamin D fortification program demonstrated a population-level impact on bone health.
- Many Australian aged care facilities have implemented standard vitamin D supplementation protocols.
Actionable Tips for Seniors and Caregivers:
- Ask your healthcare provider for a 25-hydroxyvitamin D level test.
- Typical recommended doses range from 800-2000 IU daily for seniors, but individualized dosing is crucial.
- Take vitamin D supplements with food containing some fat for better absorption.
- Consider seasonal adjustments, potentially taking higher doses in winter and lower doses in summer.
- Combine vitamin D supplementation with weight-bearing exercise for maximum benefit to bone and muscle health.
Why Vitamin D Supplementation Deserves Its Place in Fall Prevention:
Addressing vitamin D deficiency is a relatively simple and cost-effective intervention that can significantly improve muscle strength and bone health in seniors. While research on its direct impact on fall prevention is ongoing, the potential benefits, particularly for those with deficiencies, coupled with its role in overall health, warrant its inclusion in any comprehensive fall prevention plan. For Caring Hands Senior Services clients, vitamin D assessments and appropriate supplementation can be a valuable part of their personalized care plan, promoting their well-being and reducing their risk of falls.
8. Assistive Technology and Wearable Devices
Assistive technology and wearable devices offer a modern approach to preventing falls in the elderly. These solutions leverage advancements in sensor technology, artificial intelligence, and communication systems to provide both preventative measures and rapid emergency response. This technology acts as an added layer of safety, allowing seniors to maintain their independence while mitigating the risks associated with falls. They work by continuously monitoring the individual, detecting falls as they happen, and automatically alerting designated contacts or emergency services. Some advanced systems can even predict an increased risk of falling based on changes in gait or balance, allowing for proactive intervention.

From personal emergency response systems (PERS) to smart home integrations, the range of options caters to various needs and levels of tech-savviness. PERS devices, like Philips Lifeline with AutoAlert, are equipped with fall detection capabilities and can automatically summon help if a fall is detected. Wearable sensors, like those found in the Apple Watch or specialized smart belts like Tango, can monitor gait and balance metrics, even predicting potential falls before they occur. Smart home systems can be configured with motion detection and automated lighting to minimize fall risks in the home environment. Furthermore, hip protectors can offer a crucial layer of protection against fractures during a fall. For a more clinical approach, platforms like ZIBRIO and SafeStep provide in-depth balance and gait assessments, often used by healthcare professionals to tailor fall prevention strategies.
Pros:
- Continuous Monitoring: Provides 24/7 monitoring without requiring constant human presence.
- Immediate Alerts: Ensures rapid response in the event of a fall.
- Predictive Capabilities: Some systems can identify increased fall risk before incidents occur.
- Integration: Can integrate with other health monitoring systems for a comprehensive overview.
- User-Friendly Designs: Modern devices are becoming increasingly discreet and user-friendly, reducing stigma.
Cons:
- Cost: Initial investment and ongoing subscription fees can be a barrier.
- Technology Adoption: Some elderly individuals may face challenges adapting to new technology.
- Privacy Concerns: Continuous monitoring raises legitimate privacy considerations.
- False Alarms: Systems can sometimes generate false alarms, leading to unnecessary anxiety.
- False Sense of Security: Technology should complement, not replace, addressing underlying fall risks.
Tips for Choosing and Implementing Assistive Technology:
- Simplicity: Opt for devices with user-friendly interfaces and minimal maintenance requirements.
- Regular Testing: Test emergency response systems frequently to ensure they are functioning correctly.
- Comfort: Choose wearables that are comfortable for continuous use.
- Family Monitoring: Consider systems that allow family members to receive alerts and monitor activity.
- Water Resistance: Look for water-resistant devices for bathroom use, a common location for falls.
Why This Deserves a Place on the List: Falls are a significant health concern for seniors, often leading to serious injuries and reduced independence. Assistive technology provides a valuable tool for mitigating this risk, offering a proactive and reactive approach to fall prevention. This technology empowers seniors to maintain an active lifestyle while providing peace of mind for both themselves and their families. For family caregivers, these tools provide a crucial safety net, especially when constant supervision is not feasible. This makes assistive technology a vital component of any comprehensive fall prevention strategy. These technologies are particularly relevant to Caring Hands Senior Services target demographics of seniors, family caregivers, and healthcare professionals, offering solutions for aging in place, respite care, and post-discharge support. They also address the needs of Medicaid beneficiaries seeking accessible and effective fall prevention solutions.
Fall Prevention Strategies: Key Feature Comparison
| Strategy | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Strength and Balance Training Programs | Moderate – requires supervision and consistency | Moderate – professional guidance, equipment | Significant improvement over weeks; reduces fall risk | Elderly with mild to moderate mobility issues; group or individual exercise | Improves strength, coordination, and reaction time; adaptable to levels; social benefits |
| Medication Review and Management | Moderate to High – requires coordination among providers | Moderate – healthcare professional time | Immediate to short-term risk reduction | Older adults on multiple medications or with side-effect risks | Addresses modifiable medication risks; improves overall health; cost-saving |
| Home Safety Modifications | Low to Moderate – professional assessments may be needed | Variable – cost of modifications and possibly installation | Long-term passive reduction in home fall hazards | Seniors living at home, especially with environmental fall risks | One-time changes with lasting effect; low ongoing effort; enables aging in place |
| Vision Assessment and Correction | Moderate – requires specialist visits and possible surgery | Moderate – specialist care, corrective devices | Immediate to medium-term improvement | Seniors with vision impairments affecting balance and spatial awareness | Addresses a major overlooked risk; improves quality of life; often insurance covered |
| Footwear Assessment and Modification | Low – relatively simple to perform | Low to Moderate – cost of shoes and orthotics | Immediate improvement in stability | Elderly with improper or worn footwear; foot pain or gait issues | Cost-effective; improves comfort and mobility; directly affects balance |
| Multifactorial Fall Risk Assessment and Intervention | High – multidisciplinary coordination needed | High – multiple providers, assessments, interventions | Moderate reduction (~24%) in falls; personalized care | Complex cases with multiple fall risk factors | Comprehensive and individualized; coordinates care; detects hidden issues |
| Vitamin D Supplementation | Low – simple to implement with testing | Low – supplements and blood tests | Moderate benefit, mostly for deficient individuals | Seniors with confirmed vitamin D deficiency | Low cost; minimal side effects; benefits bone and muscle health |
| Assistive Technology and Wearable Devices | Moderate to High – device setup and monitoring | Moderate to High – technology cost and maintenance | Immediate fall detection and potential fall risk prediction | Seniors living alone or at high fall risk; needing monitoring support | Continuous monitoring; emergency alerts; predictive capabilities; integrates with health systems |
Taking Proactive Steps for a Safer Future
Preventing falls in the elderly is not merely a health concern; it's about preserving independence, dignity, and quality of life. This article has highlighted key strategies, from strength and balance training and medication management to home modifications and utilizing assistive technology. By addressing these factors comprehensively, we can significantly reduce the risk of falls and their devastating consequences. Remember, the most important takeaway is that proactive intervention is key. Implementing even a few of these changes can make a dramatic difference in an elderly individual's safety and well-being, empowering them to live more confidently and fully.
Taking the next step towards fall prevention can feel overwhelming, but it doesn't have to be. For personalized support and expert guidance in navigating these crucial steps for preventing falls in elderly loved ones, Caring Hands Senior Services offers comprehensive resources and tailored care plans. Visit Caring Hands Senior Services to learn how we can help create a safer and more supportive environment, promoting independence and peace of mind for seniors and their families.

